What Can Cause Posterior Tibial Tendon Dysfunction ?
Overview
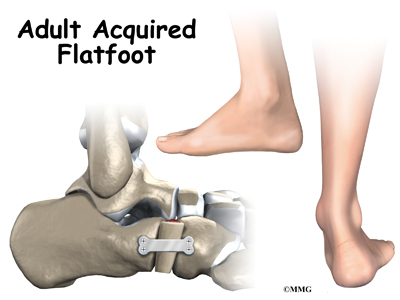
PTTD is a condition of degeneration and dysfunction in the tendon complex that helps control the medial arch of your foot. Essentially what happens is the complex is unable to do its job of supporting the arch and supinating the foot, so a progressive flat foot develops (usually called adult acquired flat foot). Initially pain and often swelling develops on the inside of the ankle and it will continue to get progressively worse. There are a number of stages of PTTD (3 Stages) and it needs to be aggressively treated early on otherwise a surgical reconstruction of the arch will invariably be required. PTTD can develop into a very disabling condition if it is not dealt with properly and promptly. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. Arthritis often develops in the foot and In more severe cases, arthritis may also develop in the ankle. 
Causes
A person with flat feet has greater load placed on the posterior tibial tendon which is the main tendon unit supporting up the arch of the foot. Throughout life, aging leads to decreased strength of muscles, tendons and ligaments. The blood supply diminishes to tendons with aging as arteries narrow. Heavier, obese patients have more weight on the arch and have greater narrowing of arteries due to atherosclerosis. In some people, the posterior tibial tendon finally gives out or tears. This is not a sudden event in most cases. Rather, it is a slow, gradual stretching followed by inflammation and degeneration of the tendon. Once the posterior tibial tendon stretches, the ligaments of the arch stretch and tear. The bones of the arch then move out of position with body weight pressing down from above. The foot rotates inward at the ankle in a movement called pronation. The arch appears collapsed, and the heel bone is tilted to the inside. The deformity can progress until the foot literally dislocates outward from under the ankle joint.
Symptoms
Posterior tibial tendon insufficiency is divided into stages by most foot and ankle specialists. In stage I, there is pain along the posterior tibial tendon without deformity or collapse of the arch. The patient has the somewhat flat or normal-appearing foot they have always had. In stage II, deformity from the condition has started to occur, resulting in some collapse of the arch, which may or may not be noticeable. The patient may feel it as a weakness in the arch. Many patients initially present in stage II, as the ligament failure can occur at the same time as the tendon failure and therefore deformity can already be occurring as the tendon is becoming symptomatic. In stage III, the deformity has progressed to the extent where the foot becomes fixed (rigid) in its deformed position. Finally, in stage IV, deformity occurs at the ankle in addition to the deformity in the foot.
Diagnosis
Clinicians need to recognize the early stage of this syndrome which includes pain, swelling, tendonitis and disability. The musculoskeletal portion of the clinical exam can help determine the stage of the disease. It is important to palpate the posterior tibial tendon and test its muscle strength. This is tested by asking patient to plantarflex and invert the foot. Joint range of motion is should be assessed as well. Stiffness of the joints may indicate longstanding disease causing a rigid deformity. A weightbearing examination should be performed as well. A complete absence of the medial longitudinal arch is often seen. In later stages the head of the talus bone projects outward to the point of a large "lump" in the arch. Observing the patient's feet from behind shows a significant valgus rotation of the heel. From behind, the "too many toes" sign may be seen as well. This is when there is abducution of the forefoot in the transverse plane allowing the toes to be seen from behind. Dysfunction of the posterior tibial tendon can be assessed by asking the patient to stand on his/her toes on the affected foot. If they are unable to, this indicates the disease is in a more advanced stage with the tendon possibly completely ruptured.
Non surgical Treatment
Initial treatment is based on the degree of deformity and flexibility at initial presentation. Conservative treatment includes orthotics or ankle foot orthoses (AFO) to support the posterior tibial tendon (PT) and the longitudinal arch, anti-inflammatories to help reduce pain and inflammation, activity modification which may include immobilization of the foot and physical therapy to help strengthen and rehabilitate the tendon. 
Surgical Treatment
When conservative care fails to control symptoms and/or deformity, then surgery may be needed. The goal of surgical treatment is to obtain good alignment while keeping the foot and ankle as flexible as possible. The most common procedures used with this condition include arthrodesis (fusion), osteotomy (cutting out a wedge-shaped piece of bone), and lateral column lengthening. Lateral column lengthening involves the use of a bone graft at the calcaneocuboid joint. This procedure helps restore the medial longitudinal arch (arch along the inside of the foot). A torn tendon or spring ligament will be repaired or reconstructed. Other surgical options include tendon shortening or lengthening. Or the surgeon may move one or more tendons. This procedure is called a tendon transfer. Tendon transfer uses another tendon to help the posterior tibial tendon function more effectively. A tendon transfer is designed to change the force and angle of pull on the bones of the arch. It's not clear yet from research evidence which surgical procedure works best for this condition. A combination of surgical treatments may be needed. It may depend on your age, type and severity of deformity and symptoms, and your desired level of daily activity.
Pain In The Arch Of The Foot When Running
Plantar fasciitis is a common, painful foot condition. Patients, and sometimes doctors often confuse the terms plantar fasciitis and heel spurs. Plantar fasciitis refers to the syndrome of inflammation of the band of tissue that runs from the heel along the arch of the foot; a heel spur is a hook of bone that can form on the heel bone (calcaneus). About 70% of patients with plantar fasciitis have been noted to have a heel spur that can be seen on x-ray.

Causes
The arch of the foot is a very complex structure, consisting of multiple bones and ligaments. Most causes of arch pain are related to the anatomy of the arch and the types of physical activity that you perform. For example, a classic set up for arch pain is people who engage in lots of high impact exercise (such as running) while wearing a type of athletic shoe that does not properly support their type of foot arch.
Symptoms
The most common symptoms of plantar fasciitis include pain on the bottom of the foot near the heel, pain with the first few steps after getting out of bed in the morning, or after a long period of rest, such as after a long car ride. The pain subsides after a few minutes of walking. Greater pain after (not during) exercise or activity.
Diagnosis
Diagnosis of a plantar plate tear can often be challenging due to the complex nature of the anatomy of the foot. Careful history taking and an examination of the area of pain is required to determine the extent and cause of the tear. If necessary, further investigations such as x-rays or diagnostic ultrasound may be ordered by your podiatrist to help evaluate the severity of the problem.
Non Surgical Treatment
The most effective treatment for foot arch pain and strain is to use an arch support. The arch support sits under the foot and stops the arch of the foot from collapsing, thereby preventing the stretch of the arch pad which causes pain and discomfort. Wearing an arch support in slippers or house shoes can also prevent pain in the mornings when discomfort it most common and severe. Arch supports usually relieve symptoms within a few days.

Surgical Treatment
The soft tissue surgeries usually would include a lengthening of the Achilles tendon, releasing of the plantar fascia as well as tendon transfers. These procedures are usually done in conjunction with bony procedures such as calcaneal osteotomies (to lower the heel bone and get it more under the leg itself), as well as metatarsal osteotomies. These procedures usually involve either cutting or fusion of the bones, and placement of fixation devices to allow the bones to heal. Healing time is usually at least 6-8 weeks and usually the patient must be non-weight bearing during the healing process. These types of surgical corrections are usually reserved for the more difficult, painful and deformed feet. They can require more surgeries down the line. These procedures are usually the last resort after all other modes of treatment have been exhausted (except in children where it is usually best to treat the deformity early). There are many different degrees of high arched feet and these procedures should be left for the more extreme cases. These cases usually require a very high degree of surgical skill and should only be done by those who frequently perform these types of cases.
Stretching Exercises
Gastroc stretch. Stand on the edge of a step. Rise slowly on your toes. Lower yourself slowly as far as you can until you feel a stretch in your calf. Don?t roll your foot inward or outward. Hold for 1-2 seconds. Reps:10-20 (stop before you fatigue). Soleus stretch. Same as above, but start with your knee bent so that you feel a slight stretch in your calf or achilles. Maintain the angle of your knee throughout the stretch. Bicycle stretch. Lie on your side. Keeping your top leg straight, bring your knee toward your nose until you feel a slight stretch in the hamstring. Maintaining this angle at your hip, start pretending you are pedalling a bicycle with the top leg. Make sure you feel a slight stretch each time your knee is straight. Reps: 10-30 for each leg. If you feel any pops or clicks in your hip or back, try raising the top leg a little (making the thighs further apart) to eliminate the popping. Foot Intrinsic Exercises. Assisted metatarsal head raising. Sit in a chair. Find the bumps at the ball of your foot just before your big toe and just before the little toe. These are the first (big toe) and fifth (little toe) metatarsal heads. Place your second and third fingers from one hand under the first metatarsal head, and the second and third fingers from the other hand under the fifth metatarsal head. Now lay the thumbs from each hand in a diagonal across your toes so that they form a right angle meeting at the nail of the second toe. Your hands are now in position to assist your toes. Keep your toes straight, with the toe pads on the floor. Use your fingers to help raise all the metatarsal heads (the ball of your foot). Do not let your toes curl under keep them long. Now relax. Reps 7-10 for each foot. As this exercise gets easier, let your fingers do less of the work until your toes can do the exercise unassisted. This can take up to three weeks. When your strength has improved to this point, you can progress to the following three exercises, which are best done in stocking feet on a slippery floor. Active metatarsal head raising. Stand with your weight on both feet. Raise your metatarsal heads (the ball of your foot) while keeping your toes from curling under and maintaining your heel on the ground. Relax. Reps 6-7. Do one foot at a time. If you do more reps than you are ready for, you may well develop cramping in your foot. I once had a client who thought if seven reps were good, 10 were better. For good measure, she did the 10 reps 10 times in a day, and then she was unable to walk the next day from having used a set of muscles she had never exercised before. Don?t overdo it.
Achilles Tendon Rupture Repair With Flexor Hallucis Longus Muscle
Overview  The exact number of people who develop Achilles tendon injury is not known, because many people with mild tendonitis or partial tear do not seek medical help. It is believed to be more common in men but with the recent participation of women in athletics, the incidence of Achilles tendon injury is also increasing in this population. Overall, injury to the Achilles tendon is by far most common in the athlete/active individual. Causes The Achilles tendon is most commonly injured by sudden plantarflexion or dorsiflexion of the ankle, or by forced dorsiflexion of the ankle outside its normal range of motion. Other mechanisms by which the Achilles can be torn involve sudden direct trauma to the tendon, or sudden activation of the Achilles after atrophy from prolonged periods of inactivity. Some other common tears can occur from overuse while participating in intense sports. Twisting or jerking motions can also contribute to injury. Fluoroquinolone antibiotics, famously ciprofloxacin, are known to increase the risk of tendon rupture, particularly achilles. Symptoms When the Achilles tendon ruptures a loud bang or popping sound may be heard. The person may feel that they have been hit or kicked in the back of the lower leg and often they will look over their shoulder to see who or what has hit them. This is quickly followed by the sudden onset of sharp pain in the tendon and a loss of strength and function. If a complete rupture has occurred it may not be possible to lift the heel off the ground or point the toes. Often the degree of pain experienced, or lack of it, can be inversely proportional to the extent of the injury, ie a partial rupture may in fact be more painful than a complete rupture. Diagnosis Laboratory studies usually are not necessary in evaluating and diagnosing an Achilles tendon rupture or injury, although evaluation may help to rule out some of the other possibilities in the differential diagnosis. Plain radiography. Radiographs are more useful for ruling out other injuries than for ruling in Achilles tendon ruptures. Ultrasonography of the leg and thigh can help to evaluate the possibility of deep venous thrombosis and also can be used to rule out a Baker cyst, in experienced hands, ultrasonography can identify a ruptured Achilles tendon or the signs of tendinosis. Magnetic resonance imaging (MRI). MRI can facilitate definitive diagnosis of a disrupted tendon and can be used to distinguish between paratenonitis, tendinosis, and bursitis. Non Surgical Treatment The other option is to allow your tendon to heal without surgery. In this case, you also need to wear a cast, splint, walking boot, or brace for 6-8 weeks. You also may have different exercises to do. If you are less active or have a chronic illness that prevents surgery, this option may be better for you.
The exact number of people who develop Achilles tendon injury is not known, because many people with mild tendonitis or partial tear do not seek medical help. It is believed to be more common in men but with the recent participation of women in athletics, the incidence of Achilles tendon injury is also increasing in this population. Overall, injury to the Achilles tendon is by far most common in the athlete/active individual. Causes The Achilles tendon is most commonly injured by sudden plantarflexion or dorsiflexion of the ankle, or by forced dorsiflexion of the ankle outside its normal range of motion. Other mechanisms by which the Achilles can be torn involve sudden direct trauma to the tendon, or sudden activation of the Achilles after atrophy from prolonged periods of inactivity. Some other common tears can occur from overuse while participating in intense sports. Twisting or jerking motions can also contribute to injury. Fluoroquinolone antibiotics, famously ciprofloxacin, are known to increase the risk of tendon rupture, particularly achilles. Symptoms When the Achilles tendon ruptures a loud bang or popping sound may be heard. The person may feel that they have been hit or kicked in the back of the lower leg and often they will look over their shoulder to see who or what has hit them. This is quickly followed by the sudden onset of sharp pain in the tendon and a loss of strength and function. If a complete rupture has occurred it may not be possible to lift the heel off the ground or point the toes. Often the degree of pain experienced, or lack of it, can be inversely proportional to the extent of the injury, ie a partial rupture may in fact be more painful than a complete rupture. Diagnosis Laboratory studies usually are not necessary in evaluating and diagnosing an Achilles tendon rupture or injury, although evaluation may help to rule out some of the other possibilities in the differential diagnosis. Plain radiography. Radiographs are more useful for ruling out other injuries than for ruling in Achilles tendon ruptures. Ultrasonography of the leg and thigh can help to evaluate the possibility of deep venous thrombosis and also can be used to rule out a Baker cyst, in experienced hands, ultrasonography can identify a ruptured Achilles tendon or the signs of tendinosis. Magnetic resonance imaging (MRI). MRI can facilitate definitive diagnosis of a disrupted tendon and can be used to distinguish between paratenonitis, tendinosis, and bursitis. Non Surgical Treatment The other option is to allow your tendon to heal without surgery. In this case, you also need to wear a cast, splint, walking boot, or brace for 6-8 weeks. You also may have different exercises to do. If you are less active or have a chronic illness that prevents surgery, this option may be better for you.  Surgical Treatment Debate remains regarding the best form of treatment for a ruptured Achilles tendon. The 2 options are:immobilisation or operation. A recent meta-analysis of scientific studies showed that compared to immobilisation, an operation reduces the risk of re-rupture and allows a quicker return to work. An operation is not without risk and these must be balanced against the benefit of a lower re-rupture rate. Both treatments involve immobilisation for 8 weeks.
Surgical Treatment Debate remains regarding the best form of treatment for a ruptured Achilles tendon. The 2 options are:immobilisation or operation. A recent meta-analysis of scientific studies showed that compared to immobilisation, an operation reduces the risk of re-rupture and allows a quicker return to work. An operation is not without risk and these must be balanced against the benefit of a lower re-rupture rate. Both treatments involve immobilisation for 8 weeks.
Fallen Arches?

Flexible flatfeet are considered normal in young children because babies are not born with a normal arch. The arch may not form fully until sometime between ages 7 and 10. Even in adulthood, 15% to 25% of people have flexible flatfeet. Most of these people never develop symptoms. In many adults who have had flexible flatfeet since childhood, the missing arch is an inherited condition related to a general looseness of ligaments. These people usually have extremely flexible, very mobile joints throughout the body, not only in the feet. Flatfeet also can develop during adulthood. Causes include joint disease, such as rheumatoid arthritis, and disorders of nerve function (neuropathy). Unlike a flexible flatfoot, a rigid flatfoot is often the result of a significant problem affecting the structure or alignment of the bones that make up the foot's arch. Some common causes of rigid flatfeet include. Congenital vertical talus. In this condition, there is no arch because the foot bones are not aligned properly. In some cases, there is a reverse curve (rocker-bottom foot, in which the shape is like the bottom rails of a rocking chair) in place of the normal arch. Congenital vertical talus is a rare condition present at birth. It often is associated with a genetic disorder, such as Down syndrome, or other congenital disorders. The cause is unknown in up to half of cases. Tarsal coalition (peroneal spastic flatfoot). In this inherited condition, two or more of the foot bones are fused together, interfering with the flexibility of the foot and eliminating the normal arch. A rare condition, it often affects several generations of the same family. Lateral subtalar dislocation. Sometimes called an acquired flatfoot, it occurs in someone who originally had a normal foot arch. In a lateral subtalar dislocation, there is a dislocation of the talus bone, located within the arch of the foot. The dislocated talus bone slips out of place, drops downward and sideways and collapses the arch. It usually occurs suddenly because of a high-impact injury related to a fall from a height, a motor vehicle accident or participation in sports, and it may be associated with fractures or other injuries.
Causes
Family history, experts say fallen arches can run in families. Weak arch, the arch of the foot may be there when no weight is placed on it, for example, when the person is sitting. But as soon as they stand up the foot flattens (falls) onto the ground. Injury, arthritis, tibialis posterior (ruptured tendon), pregnancy, nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Tarsal Coalition, the bones of the foot fuse together in an unusual way, resulting in stiff and flat feet. Most commonly diagnosed during childhood. Diabetes. Age and wear and tear, years of using your feet to walk, run, and jump eventually may take its toll. One of the eventual consequences could be fallen arches. The posterior tibial tendon may become weakened after long-term wear a tear. The postario tibial tendon is the main support structure of the arch of our feet. The tendon can become inflamed (tendinitis) after overuse - sometimes it can even become torn. Once the tendon is damaged, the arch shape of the foot may flatten.
Symptoms
People will have a very heavily dropped arch and it won?t affect them at all and people will have it slightly dropped and it could cause fierce problems. It could cause things like plantar fasciitis, it could cause heel spurs, desperate ball-of-the-foot pressure, or pressure on the big toe known as the hallux which causes discomfort in the foot. It will create problems upwards to the knees, hips and the back once you?re out of line.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
Non Surgical Treatment
Some patients with flat feet may automatically align their limbs in such a way that unpleasant symptoms never develop. In such cases treatment is not usually required. Pain in the foot that is caused by flat feet may be alleviated if the patient wears supportive well-fitted shoes. Some patients say that symptoms improve with extra-wide fitting shoes. Fitted insoles or orthotics (custom-designed arch supports) may relieve pressure from the arch and reduce pain if the patient's feet roll or over-pronate. The benefits of an orthotic only exist while it is being worn. Patients with tendonitis of the posterior tibial tendon may benefit if a wedge is inserted along the inside edge of the orthotic - this takes some of the load off the tendon tissue. Wearing an ankle brace may help patients with posterior tibial tendinitis, until the inflammation comes down. Rest, doctors may advise some patients to rest and avoid activities which may make the foot (feet) feel worse, until the foot (feet) feels better. A combination of an insole and some kind of painkiller may help patients with a ruptured tendon, as well as those with arthritis. Patients with a ruptured tendon or arthritis who find insoles with painkillers ineffective may require surgical intervention. Patients, usually children, whose bones did not or are not developing properly, resulting in flat feet from birth, may require surgical intervention to separate fused bones (rare). Bodyweight management, if the patient is obese the doctor may advise him/her to lose weight. A significant number of obese patients with flat feet who successfully lose weight experience considerable improvement of symptoms.
Surgical Treatment

Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Sit up straight in a chair with your feet flat on the ground. Scrunch up the toes of one foot as if you are trying to grab hold of the floor then use your toes to drag your foot a small distance forwards. Do this a couple of times on each foot, but don?t use your leg muscles to push your foot forward -- the movement should come solely from the muscles in your feet. Sit in a chair and place a cleaning cloth, towel or small ball on the floor at your feet. Use the toes of one foot to grasp the object and lift it off the floor. This action will require you to clench your toes and contract your arch. Once you have lifted the object a little way off the floor, try to throw it in the air and catch it by stretching your toes and arch out and upwards. Repeat the exercise several times on both feet. Sit on the floor with your legs straight out in front of you then bend your knees out to either side and place the soles of your feet together so your legs form a diamond. Hold on to your ankles and, keeping your heels together at all times, separate your feet so your toes point out to either side. Open and close your feet in this way several times, making sure your little toes stay in contact with the floor throughout the exercise. Starting in the same position, try separating your heels, keeping your toes together at all times.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Pain In The Arches Everything You Need To Know
Plantar fasciitis can be a real pain in the foot. Plantar fasciitis is the medical term for inflammation of the plantar fascia, which is the connective tissue that runs along the bottom of your foot. If you?ve ever had pain in the bottom of your foot with the first few steps out of bed in the morning, you?ve probably had some experience with this painful condition. In active populations, plantar fasciitis is often associated with overuse or a sudden change in activity, and temporarily easing off of activity can be part of the solution. In more sedentary populations, weight gain is usually a major contributor to plantar fasciitis and a weight-loss plan could be of benefit. Whether you?re active or sedentary, however, previous foot injuries, poor arch support, or tight muscles around the foot can all predispose you to plantar fasciitis.

Causes
Plantar fasciitis, another sports injury detailed on this website, is regularly the cause of foot arch pain or strain. This can arise due to faulty biomechanics in your feet, which alone can also provoke foot arch pains. The most prominent biomechanical difficulties are flat feet and high arches. With flat feet (or overpronation) the arches appear to be almost flattened, causing unevenness by forcing the feet roll inwards in order to maintain balance and support the body's weight. This places inordinate pressure on the plantar fascia and arches. If by contrast you have high arches (instep), the ankle can roll outwards, again causing undue strain on the arches. Too much of this strain can lead to stretching of the plantar fascia and pain in the arches. Other causes include overstretching or otherwise pressuring the arches, for example by exercising with fatigued leg muscles which leave the feet with excessive work to do. You are also particularly at risk if in your 40s or 50s and commencing an intense program of training after a long period of inactivity.
Symptoms
Go to a podiatrist at the first sign of symptoms. Besides pain on the bottom of the foot, additional symptoms may include. Burning sensation in arch. Difficulty standing on tiptoes. Inflammation. More pain after sleeping or resting. Redness. Heat. Localized pain in the ball of the foot. Sharp or shooting pain in the toes. Pain that increases when toes are flexed. Tingling or numbness in the toes. Aching. Pain that increases when walking barefoot. Pain that increases when walking on hard surfaces. Pain the increases when standing (putting weight on your feet) or moving around and decreases when immobile. Skin Lesions. It?s important to get a proper diagnosis and treatment plan. Let?s go over the possible causes of the pain.
Diagnosis
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs. A high arch. An area of maximum tenderness on the bottom of your foot, just in front of your heel bone. Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down. Limited "up" motion of your ankle.
Non Surgical Treatment
Relieving the pain caused by plantar fasciitis boils down to two basic needs. Reduce the inflammation. Support and stretch the plantar fascia. If you can accomplish those two goals, you should note pain relief more quickly. Doctors treating plantar fasciitis will recommend the following options for accomplishing this. Rest, Get off your feet as much as possible when the pain is at its worst. If you must walk or run, try to stay off hard, unforgiving surfaces and wear supporting footwear. Use ice on the arch several times a day to help reduce swelling if necessary. Take Tylenol, Advil, or other over-the-counter pain relievers that contain acetaminophen, ibuprofen, or naproxen to help lessen the inflammation and ease pain. Stretch your toes, calves, and foot repeatedly throughout the day to keep the plantar fasciia limber. Purchase insoles, inserts, or orthopedic shoes designed to support the arch of the foot and wear them at all times. Purchase splints that will stretch the Achilles tendon as you sleep, helping to lessen morning heel pain. If none of the above helps, your doctor may prescribe regular injections of cortisone to control the pain. As a last resort, your doctor may attempt surgery to repair the plantar fascia.

Surgical Treatment
In cases where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The goal of surgery and non-surgical treatment is to eliminate pain, stop progression of the deformity and improve mobility of the patient. Opinions vary as to the best surgical treatment for adult acquired flatfoot. Procedures commonly used to correct the condition include tendon debridement, tendon transfers, osteotomies (cutting and repositioning of bone) and joint fusions.
Prevention
To prevent arch pain, it is important to build up slowly to your exercise routine while wearing arch supports inside training shoes. By undertaking these simple measures you can prevent the discomfort of arch pain which can otherwise linger for many months. While you allow the foot to recover, it will help to undertake low impact exercises (such as swimming or water aerobics).
The Brings About Of Adult Aquired Flat Feet ?
The posterior tibial tendon can serve as among your significant supporting structures with the foot, helping it to work whilst walking. Posterior tibial tendon dysfunction (PTTD) is really a situation due to changes inside the tendon, impairing its ability to keep the arch. This leads to flattening with the foot. PTTD is often known as ?adult acquired flatfoot? since it may end up being the most typical type involving flatfoot developed in the particular program of adulthood. Even though this issue typically occurs in only one foot, some individuals might develop it within both feet. PTTD is usually progressive, which means it will keep obtaining worse, particularly if it isn?t treated early.

Causes
Rheumatoid arthritis This kind of type regarding arthritis attacks the particular cartilage within the foot, ultimately causing pain and flat feet. The idea will be due to auto-immune disease, in which the body?s disease fighting capability attacks its extremely own tissues. Diabetes. having diabetes may cause nerve damage as well as affect the feeling within your feet and also trigger arch collapse. Bones could furthermore fracture but some patients might not feel any kind of pain because of for the nerve damage. Weight Problems and/or hypertension (high blood pressure) This specific increases your current risk of tendon damage and resulting flat foot.
Symptoms
Depending about the cause in the flatfoot, any patient could expertise 1 as well as more of the actual various signs here. Pain across the span of your posterior tibial tendon which in turn lies about the inside in the foot as well as ankle. This particular can be associated together with swelling on the inside in the ankle. Pain that is a whole lot worse with activity. Substantial intensity or impact activities, like running, can become very difficult. some patients can have a new problem strolling or even standing for too long durations of time. Once the foot collapses, the actual heel bone might shift position and set stress about the outside ankle bone (fibula). This kind of can cause pain about the not within the ankle. Arthritis within the heel in addition causes this exact same type associated with pain. Patients with an old injury or perhaps arthritis in the middle associated with the foot can easily possess painful, bony bumps about the leading and also inside with the foot. These kind of make shoewear really difficult. Occasionally, the bony spurs are usually consequently significant which they pinch the particular nerves which can lead to numbness along with tingling around the top of the foot and in to the toes. Diabetics may only discover swelling as well as a sizable bump on the bottom of the foot. Simply Because their particular sensation can be affected, individuals with diabetes may not need just about any pain. Your significant bump could cause skin problems as well as an ulcer (a sore that will not heal) could develop if correct diabetic shoewear just isn't used.
Diagnosis
Examination simply by your foot as well as ankle specialist could confirm the diagnosis for many patients. An ultrasound exam performed in the workplace environment can measure the status in the posterior tibial tendon, the actual tendon which can easily be primarily accountable for supporting the actual arch construction of the foot.
Non surgical Treatment
Nonoperative treatment associated with stage 1 and two acquired adult flatfoot deformity can be successful. General components in the treatment range through the use involving comfort shoes. activity modification to always be able to avoid exacerbating activities. weight loss if indicated. specific components associated with therapy which with time may lead to marked improvement within signs and symptoms incorporate a substantial repetition, reduced resistance strengthening program. Proper bracing or even a medial longitudinal arch support. When the posterior tibial tendon can be intact, a number of workout routines directed at strengthening the particular elongated along with dysfunctional tendon complex may be successful. Within stage 2 deformities, this truly is mixed having an ankle brace for any period involving time regarding 2-3 months until the actual signs resolve. In this point, the particular individual will be transitioned to a orthotic insert which may assistance to offer the arch. Throughout patients along with stage 1 deformity it could always be feasible to create use of an arch assistance immediately.
Surgical Treatment
The indications for surgery are usually persistent pain and/or significant deformity. At times the foot just feels weak as well as the assessment involving deformity is better completed by a foot and also ankle specialist. If surgery is actually appropriate, a new mix of soft tissue as well as bony procedures may always be considered for you to appropriate alignment as well as keep the medial arch, taking strain off failing ligaments. Depending upon your tissues concerned as well as extent associated with deformity, the particular foot and also ankle specialist will determine the actual essential combination of procedures. Surgical treatments may incorporate a medial slide calcaneal osteotomy for you to right position of the heel, any lateral column lengthening in order to right position in the midfoot plus a medial cuneiform osteotomy or 1st metatarsal-tarsal fusion in order to correct elevation in the medial forefoot. The Actual posterior tibial tendon might always be reconstructed with a tendon transfer. Within severe cases (stage III), your reconstruction can include fusion with the hind foot,, resulting in stiffness of the hind foot nevertheless the desired pain relief. Throughout probably the actual most severe stage (stage IV), the actual deltoid ligament about the inside with the ankle fails, resulting within the deformity within the ankle. This kind of deformity as moment passes may outcome in arthritis inside the ankle.
Pain In The Foot's Arch Causes Symptoms And Treatments
Flexible flatfeet are considered normal in young children because babies are not born with a normal arch. The arch may not form fully until sometime between ages 7 and 10. Even in adulthood, 15% to 25% of people have flexible flatfeet. Most of these people never develop symptoms. In many adults who have had flexible flatfeet since childhood, the missing arch is an inherited condition related to a general looseness of ligaments. These people usually have extremely flexible, very mobile joints throughout the body, not only in the feet. Flatfeet also can develop during adulthood. Causes include joint disease, such as rheumatoid arthritis, and disorders of nerve function (neuropathy).

Causes
A common cause of foot arch pain is a stress fracture. They tend to occur from repeated overloading of one of the foot bones from activities such as jumping and running especially if you have suddenly increased your activity level. The breaks in the bone may be small but they can be extremely painful. Stress fractures of the metatarsal bones or the navicular can cause anything from mild to severe foot arch pain. The Tibialis Posterior muscle plays a very important role in supporting the medial arch of the foot. Posterior Tibial Tendonitis can occur either through repetitive use e.g. high impact sports such as soccer or tennis, or from an injury e.g. a fall. This causes the tendon to become inflamed or even torn, resulting in pain on bottom of foot. This pain usually gets worse with activity or when standing for long periods. If the problem persists, the inner side of the foot (known as the medial longitudinal arch of the foot) gradually collapses down, causing flat feet. A simple test for this condition is to stand on one leg and rise up onto your tiptoes. If you cannot, it indicates a problem with the Posterior Tibial tendon. Treatment usually consists of rest, ice, exercises, orthotics and physical therapy.
Symptoms
Intense heel pain, especially first thing in the morning and after a long day. Difficulty walking or standing for long periods without pain. Generally, the sharp pain associated with plantar fasciitis is localized to the heel, but it can spread forward along the arch of the foot and back into the Achilles tendon. While severe cases can result in chronic pain that lasts all day, the most common flare ups occur first thing in the morning, making those first steps out of bed a form of torture, and in the evening after having spent a day on your feet. Overpronation (a foot that naturally turns too far inward), high arches, and flat feet (fallen arches) can all cause similar arch pain. In these cases, however, the pain is more likely to continue throughout the day rather than being worst in the morning.
Diagnosis
In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics.
Non Surgical Treatment
An orthotic arch support, specially molded to fit your foot, may be part of your treatment. These supports can be particularly helpful if you have flat feet or high arches. You can tell if that is what is needed when short-term taping decreases your heel pain.

Surgical Treatment
Although most patients with plantar fasciitis respond to non- surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstays of long-term treatment for plantar fasciitis.
Prevention
It is possible to prevent arch pain by wearing well-fitting shoes while performing any physical activity. Many times doctors will suggest a therapeutic shoe with a higher heel to relieve the pressure on the achilles tendon and also the arch muscle (plantar fasciitis). People with arch pain suffer from regular flare-ups of pain. However there is no risk to others as this is not a contagious condition.
Stretching Exercises
Strength training and stretching can help avoid injury and keep your feet free from pain. Stretching should focus on the bottom of your foot to loosen tissues and tight ligaments surrounding your arch. The easiest way to do this is by grabbing a towel and sitting on the floor. You can do this while you catch up on the news in the morning, or when you get home from work. Put one leg out in front with your foot flexed up. Loop the towel around the ball of your foot and gently pull your toes towards you. Hold for thirty seconds and then repeat 3-4 times before switching feet.