The Causes Of Calcaneal Spur
Overview
A heel spur is a hooked bony growth protruding from the calcaneus or heel bone. It often occurs alongside plantar fasciitis, and as such the two conditions are often confused, however they are not the same.
Causes
Diseases such as arthritis may lead to chronic inflammation in the tissue surrounding the heel and over time this can lead to the accumulation of calcium deposits. Ankylosing spondylitis, for example, is one particular form of arthritis that frequently develops along with heel spurs. This condition can damage bones all over the body and even lead to the fusion of spinal vertebrae.

Symptoms
Heel spurs may or may not cause symptoms. Symptoms are usually related to the plantar fasciitis. You may experience significant pain. Your heel pain may be worse in the morning when you first wake up or during certain activities.
Diagnosis
Diagnosis is made using a few different technologies. X-rays are often used first to ensure there is no fracture or tumor in the region. Then ultrasound is used to check the fascia itself to make sure there is no tear and check the level of scar tissue and damage. Neurosensory testing, a non-painful nerve test, can be used to make sure there is not a local nerve problem if the pain is thought to be nerve related. It is important to remember that one can have a very large heel spur and no plantar fasciitis issues or pain at all, or one can have a great deal of pain and virtually no spur at all.
Non Surgical Treatment
Heel pain may be associated with a heel spur, however the heel pain is usually due to plantar fasciitis, rather than a heel spur, so treatment is usually directed at the plantar fasciitis itself. Treatment usually involves application of ice to reduce pain and inflammation, special stretching exercises, and pain-relieving or anti-inflammatory medicines. Night splints or orthotics may be recommended. It may help to avoid the activities that aggravate pain, such as long walks and running. Surgery is very rarely recommended and only after other measures fail.
Surgical Treatment
Surgery is used a very small percentage of the time. It is usually considered after trying non-surgical treatments for at least a year. Plantar fascia release surgery is use to relax the plantar fascia. This surgery is commonly paired with tarsal tunnel release surgery. Surgery is successful for the majority of people.
Prevention
To prevent this condition, wearing properly fitted shoes with good arch support is very important. If a person is overweight, weight loss can help diminish stress on the feet and help prevent foot problems. For those who exercise frequently and intensely, proper stretching is always necessary, especially when there is an increase in activities or a change in running technique. It is not recommended to attempt to work through the pain, as this can change a mild case of heel spurs and plantar fascitis into a long-lasting and painful episode of the condition.
What Is Bursitis In The Foot?
A bursa is a fluid-filled sac. There are hundreds of deep and superficial bursae throughout the human body. They are typically located near major joints. Bursae are situated between bone and soft tissues like tendons, ligaments, muscles, and skin. They serve as a cushioning pad to absorb shock. The fluid within the sac is secreted to assist with friction-free movement as the soft tissues move across a bony area.
Causes
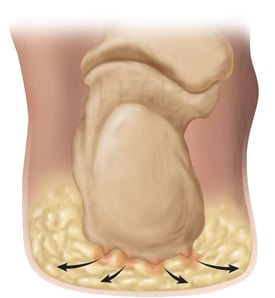
Occasionally the bursal sac can become inflamed and painful. Pain to the region is worse typically with initial weight bearing activity such as rising from bed in the morning. Swelling and warmth to the region are common. Clinical examination shows pain to palpation at the retrocalcaneus at a level just before the Achilles tendon. Increase pressure and friction of the Achilles tendon across the retrocalcaneal region is the cause of this bursitis. A high arch, tight Achilles tendon or bone spur appear to be some of the main causes of this problem. With a high arch the back portion of the calcaneus abnormally projects into the Achilles tendon region.
Symptoms
Common signs and symptoms associated with infracalcaneal bursitis include redness under the heel. Pain and swelling under the heel. Pain or ache in the middle part of the underside of the heel. Heel pain or discomfort that increases with prolonged weight-bearing activities.
Diagnosis
Plain radiographs of the calcaneus may reveal a Haglund deformity (increased prominence of the posterosuperior aspect of the calcaneus). However, on weight-bearing lateral radiographs, the retrocalcaneal recess often appears normal even in patients with retrocalcaneal bursitis, limiting its usefulness in making this diagnosis.Radiographs may be used as a diagnostic measure to support a clinician?s diagnosis of retrocalcaneal bursitis. Individuals with retrocalcaneal bursitis may have an absence of the normal radiolucency (ie, blunting) that is seen in the posteroinferior corner of the Kager fat pad, known as the retrocalcaneal recess or bursal wedge. This may occur with or without an associated erosion of the calcaneus.
Non Surgical Treatment
With posterior Achilles tendon bursitis, treatment is aimed at reducing the inflammation and adjusting the foot's position in the shoe to relieve pressure and motion on the back of the heel. Foam rubber or felt heel pads can be placed in the shoe to eliminate pressure by elevating the heel. Placing protective gel padding over the painful bursa or stretching the back part of the shoe and placing padding around the inflamed bursa may help. Sometimes a special shoe, such as a running shoe designed to stabilize the midsole heel, devices placed in the shoe (orthoses), or both can help to control abnormal foot and heel motion contributing to the posterior heel irritation. Other shoes have padding that reduces irritation to the posterior heel and Achilles tendon.
Surgical Treatment
Surgery is rarely done strictly for treatment of a bursitis. If any underlying cause is the reason, this may be addressed surgically. During surgery for other conditions, a bursa may be seen and removed surgically.
Hammer Toe Hereditary Causes
 Overview
Overview
A Hammer toes occurs when the middle of the toe points upwards abnormally. This most often occurs in the second toe, and is often the result of a big toe bunion pushing on the second toe. A painful callous often forms on top of the first joint in the toe. Treatment of a hammer toe may consist of simple padding of the callous on top of the toe, as well as buying appropriate footwear. The best shoes for patients with a hammer toe will have a wide toebox, no pressure on the end of the toe, and will not press on a bunion (which may cause worsening of the hammer toe).
Causes
Hammertoes are a contracture of the toes as a result of a muscle imbalance between the tendons on the top of the toes (extensor tendons) and the tendons on the bottom of the toes (flexor tendons). If there is an imbalance in the foot muscles that stabilize the toe, the smaller muscles can be overpowered by the larger flexor and extensor muscles.
 Symptoms
Symptoms
A soft corn, or heloma molle, may exist in the web space between toes. This is more commonly caused by an exostosis, which is basically an extra growth of bone possibly due to your foot structure. As this outgrowth of excessive bone rubs against other toes, there is friction between the toes and a corn forms for your protection.
Diagnosis
Your healthcare provider will examine your foot, checking for redness, swelling, corns, and calluses. Your provider will also measure the flexibility of your toes and test how much feeling you have in your toes. You may have blood tests to check for arthritis, diabetes, and infection.
Non Surgical Treatment
You can usually use over-the-counter cushions, pads, or medications to treat bunions and corns. However, if they are painful or if they have caused your toes to become deformed, your doctor may opt to surgically remove them. If you have blisters on your toes, do not pop them. Popping blisters can cause pain and infection. Use over-the-counter creams and cushions to relieve pain and keep blisters from rubbing against the inside of hammertoe your shoes. Gently stretching your toes can also help relieve pain and reposition the affected toe.
Surgical Treatment
If this fails or if treatment is not sought until the toes are permanently misaligned, then surgery may be required. Surgery may involve either cutting the tendon or fusing the joint. Congenital conditions should be treated in early childhood with manipulations and splinting.
 Prevention
Prevention
There should be at least one-half inch between the tip of your longest toe and the front of the shoe. Never buy shoes that feel tight and expect them to stretch with wearing. If you have prominent areas on your feet such as hammertoes and bunions, avoid shoes with a lot of stitching or multiple pieces of fabric, as these stitched areas tend not to stretch to accommodate various toe deformities.
Hammertoes Treatment At Home
 Overview
Overview
A hammertoe is a toe that's curled due to a bend in the middle joint of a toe. Mallet toe is similar, but affects the upper joint of a toe. Otherwise, any differences between hammertoe and mallet toe are subtle. Both hammertoe and mallet toe are commonly caused by shoes that are too short or heels that are too high. Under these conditions, your toe may be forced against the front of your shoe, resulting hammertoes in an unnatural bending of your toe and a hammer-like or claw-like appearance. Relieving the pain and pressure of hammertoe and mallet toe may involve changing your footwear and wearing shoe inserts. If you have a more severe case of hammertoe or mallet toe, you may need surgery to experience relief.
Causes
While there are a number of causes, there aren't many specific risk factors for hammertoes, women tend to get these problems more than men, but they occur without rhyme or reason. Diabetics, however, are more likely to get a hammertoe if they have underlying nerve damage in the toes and feet.
 Symptoms
Symptoms
The most obvious symptoms of this injury will be the the middle toe joint is permanently bent at an angle. In the beginning movement may still be possible but as time passes and the injury worsens the toe will be locked in place and possible require hammer toe correction surgery to fix. Another key indicator of hammer toe is that a lump or corn will form on top of the toe. The toe joint will be painful and walking can cause severe discomfort. Occasionally a callus may form on the sole of the injured foot. If you see any of these symptoms together or have been enduring pain for some time, seeing a podiatrist should be your next step.
Diagnosis
Hammertoes are progressive, they don?t go away by themselves and usually they will get worse over time. However, not all cases are alike, some hammertoes progress more rapidly than others. Once your foot and ankle surgeon has evaluated your hammertoes, a treatment plan can be developed that is suited to your needs.
Non Surgical Treatment
If the problem is caught in the early stages you can avoid hammer toe surgery. One of the easiest methods of treatment is to manipulate the toe out of a bent position then splint and buddy wrap it alongside it?s larger neighbour. This method of hammer toe taping will help the problem to fix itself. Make sure the toe isn?t resuming its bent shape during the recovery. To alleviate some of the painful symptoms of hammer toe avoid wearing high heels or shoes that cramp or stifle your feet. Choosing a pair of minimalist shoes can be an excellent choice for both foot and postural health. Wearing shoes that give the toes plenty of space and are comfortable lined is also a smart choice. Hammer toe recovery starts be treating the toe respectfully. Soft insoles or protection for the corn can also provide additional assistance.
Surgical Treatment
If your hammer, claw, or mallet toe gets worse, or if nonsurgical treatment does not help your pain, you may think about surgery. The type of surgery you choose depends on how severe your condition is and whether the toe joint is fixed (has no movement) or flexible (has some movement). A fixed toe joint often requires surgery to be straightened. A flexible toe joint can sometimes be straightened without surgery. Surgery choices include Phalangeal head resection (arthroplasty), in which the surgeon removes part of the toe bone. Joint fusion (arthrodesis), in which the surgeon removes part of the joint, letting the toe bones grow together (fuse). Cutting supporting tissue or moving tendons in the toe joint. How well surgery works depends on what type of surgery you have, how experienced your surgeon is, and how badly your toes are affected.
What Are The Principal Causes Of Hallux Valgus?
Overview
 When your big toe is angled towards the second toe, the deformity is called a bunion (hallux valgus). This causes a bump on the side at the base of the big toe. In addition there is often thickening of the skin and tissues next to the affected joint. The thickened skin and tissues may become inflamed, swollen and painful. Sometimes a fluid-filled sac (bursa) develops over the joint.
When your big toe is angled towards the second toe, the deformity is called a bunion (hallux valgus). This causes a bump on the side at the base of the big toe. In addition there is often thickening of the skin and tissues next to the affected joint. The thickened skin and tissues may become inflamed, swollen and painful. Sometimes a fluid-filled sac (bursa) develops over the joint.
Causes
High heels can exacerbate a potential bunion problem because they tip the body?s weight forward, forcing the toes into the front of the shoe. This may help to explain why bunions are 10 times more common in women than in men. People in occupations such as teaching and nursing, that involve a lot of standing and walking, are susceptible to bunions. Ballet dancers, whose feet suffer severe repetitive stress, are also amongst those who experience bunions. Women can sometimes develop bunions and other foot problems during pregnancy because hormonal changes loosen the ligaments and flatten the feet. Bunions are also associated with arthritis, which damages the cartilage within the joint.
Symptoms
Symptoms include pain in and around the ball of the big toe, usually from the bone rubbing too much against the shoe. You may be unable to wear certain types of shoes due to the shape of the forefoot. The big toe appears to be bent inwards towards and in come cases over the inside toe.
Diagnosis
Bunions are readily apparent, you can see the prominence at the base of the big toe or side of the foot. However, to fully evaluate your condition, the Podiatrist may arrange for x-rays to be taken to determine the degree of the deformity and assess the changes that have occurred. Because bunions are progressive, they don't go away, and will usually get worse over time. But not all cases are alike, some bunions progress more rapidly than others. There is no clear-cut way to predict how fast a bunion will get worse. The severity of the bunion and the symptoms you have will help determine what treatment is recommended for you.
Non Surgical Treatment
Most bunions can be treated without surgery. The first step for treating bunions is to ensure that your shoes fit correctly. Often good footwear is all that is needed to alleviate the problem. Shoes that are wide enough to avoid pressure on the bunion are the obvious first step. Look for shoes with wide insteps and broad toes and definitely no high heels. Sometimes, you can get your existing shoes stretched out by a shoe repairer. Seek advice from a podiatrist. Pads and toe inserts. Protective bunion pads may help to cushion the joint and reduce pain. Toe inserts are available that splint the toes straight. It may be recommended that you wear some orthotics to improve your foot position when walking. Medicines. Some people find anti-inflammatory medicines, such as ibuprofen or aspirin, or paracetamol help ease the pain of their bunions. 
Surgical Treatment
Pain is the commonest indication for bunion surgery. You may also notice redness and inflammation and usually this means that the bunion has progressed to a point that it will not respond to simple modification in shoe wear. Eventually that major joint of the big toe will become stiff and this makes it difficult for activities such as climbing stairs and sports.
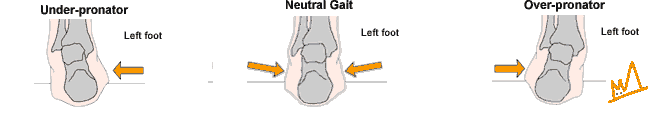
Overpronation Pain And Discomfort
One of the most common causes of foot and leg discomfort is a condition known as overpronation. Normal pronation, or "turning inward" of the foot is necessary as the foot adapts to the ground. With over pronation, the arch flattens, collapses, and soft tissues stretch. This causes the joint surfaces to function at unnatural angles to each other. When this happens, joints that should be stable now become very loose and flexible. At first, over pronation may cause fatigue. As the problem gets worse, strain on the muscles, tendons, and ligaments of the foot and lower leg can cause permanent problems and deformities.
Causes
You do not have to be a runner or athlete to suffer from overpronation. Flat feet can be inherited, and many people suffer from pain on a day-to-day basis. Flat feet can also be traumatic in nature and result from tendon damage over time. Wearing shoes that do not offer enough arch support can also contribute to overpronation.
Symptoms
When standing, your heels lean inward. When standing, one or both of your knee caps turn inward. Conditions such as a flat feet or bunions may occur. You develop knee pain when you are active or involved in athletics. The knee pain slowly goes away when you rest. You abnormally wear out the soles and heels of your shoes very quickly.
Diagnosis
A quick way to see if you over-pronate is to look for these signs. While standing straight with bare feet on the floor, look so see if the inside of your arch or sole touches the floor. Take a look at your hiking or running shoes; look for wear on the inside of the sole. Wet your feet and walk on a surface that will show the foot mark. If you have a neutral foot you should see your heel connected to the ball of your foot by a mark roughly half of width of your sole. If you over-pronate you will see greater than half and up to the full width of your sole.

Non Surgical Treatment
Anti-Pronation Insoles provide a unique foot support system that aligns the lower body. The major cause of foot and leg pain is over pronation (rolling over of the feet) which causes excessive pressure on the muscles, ligaments and bones of the lower body. Running insoles treat the underlying cause of over pronation and prevent future occurrences of the associated foot or leg condition. A project conducted at the NIKE Sport Research Laboratory studied the effects of orthotics on rear foot movement in running. Nine well-trained runners who wore orthotics were chosen as subjects. The results of the study indicated that orthotics reduced rear foot movement by roughly one degree or approximately nine percent of the amount found in runners not using orthotics. The average reduction of the maximum velocity of pronation was fifteen percent. Thus this study indicates that orthotics and insoles control over pronation which will treat and prevent many sporting injuries.
Surgical Treatment
Subtalar Arthroereisis. Primary benefit is that yje surgery is minimally invasive and fully reversible. the primary risk is a high chance of device displacement, generally not tolerated in adults.
An implant is pushed into the foot to block the excessive motion of the ankle bone. Generally only used in pediatric patients and in combination with other procedures, such as tendon lengthening. Reported removal rates vary from 38% - 100%, depending on manufacturer.
How To Diagnose Calcaneal Apophysitis?
Sever's disease is a pain that occurs in the back of the heel of physically active children at around the time of puberty. Sever's disease occurs due to an inflammation of the growth plate due to excessive pull of the achilles tendon on this growth plate. During puberty the bones quite often grow faster than the muscles and tendons causing the tendons to become tight, this tightness then results in excessive pull on the back of the heel resulting in this painful condition.
Causes
The heel bone grows faster than the ligaments in the leg. As a result, muscles and tendons can become very tight and overstretched in children who are going through growth spurts. The heel is especially susceptible to injury since the foot is one of the first parts of the body to grow to full size and the heel area is not very flexible. Sever?s disease occurs as a result of repetitive stress on the Achilles tendon. Over time, this constant pressure on the already tight heel cord can damage the growth plate, causing pain and inflammation. Such stress and pressure can result from sports that involve running and jumping on hard surfaces (track, basketball and gymnastics). Standing too long, which puts constant pressure on the heel. Poor-fitting shoes that don?t provide enough support or padding for the feet. Overuse or exercising too much can also cause Sever?s disease.
Symptoms
The main symptom of sever's disease is pain and tenderness at the back of the heel which is made worse with physical activity. Tenderness will be felt especially if you press in or give the back of the heel a squeeze from the sides. There may be a lump over the painful area. Another sign is tight calf muscles resulting with reduced range of motion at the ankle. Pain may go away after a period of rest from sporting activities only to return when the young person goes back to training.
Diagnosis
You may have pain when your doctor squeezes your heel bone. You may have pain when asked to stand or walk on your toes or on your heels. You may have pain in your heel when your doctor stretches your calf muscles. Your doctor may order x-rays of the injured foot to show an active growth plate.
Non Surgical Treatment
Treatment may consist of one or more of the following, Elevating the heel, Stretching hamstring and calf muscles 2-3 times daily, Using R.I.C.E. (Rest, Ice, Compression, Elevation), Foot orthotics, Medication, Physical therapy, Icing daily (morning), Heating therapy, Open back shoe are best and avoid high heel shoe. The Strickland Protocol has shown a positive response in patients with a mean return to sport in less than 3 weeks.
Prevention
To prevent recurrence, patients, parents, coaches, and trainers should be instructed regarding a good preexercise stretching program for the child. Early in the season, encouragement should be given for a preseason conditioning and stretching program. Coaches and trainers should be educated about recognition of the clinical symptoms so they are able to initiate early protective measures and seek medical referral when necessary.